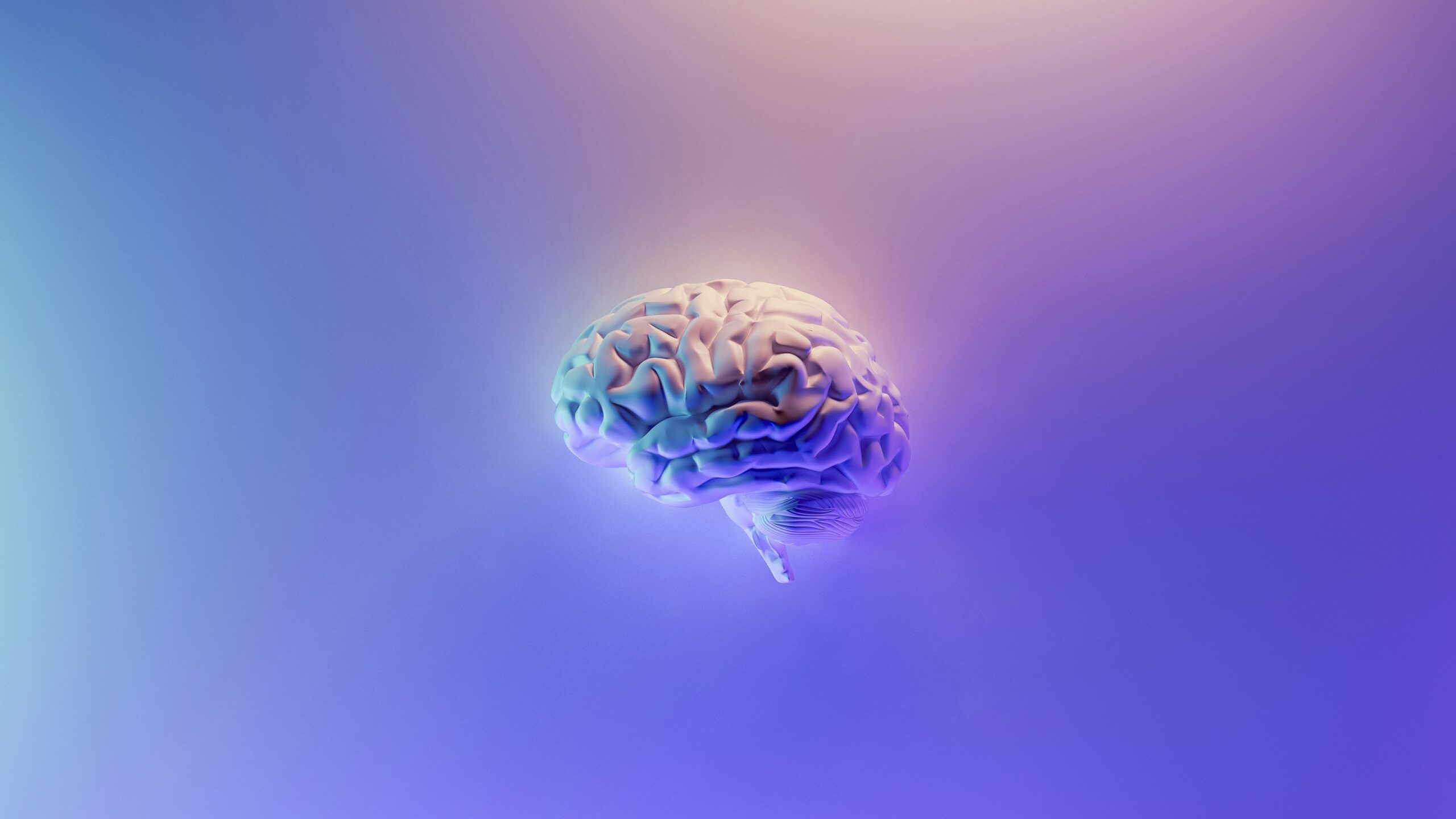
Ongoing research explores how viral infections like SARS-CoV-2 impact brain function, offering hope for understanding and treating long-term cognitive issues
Long COVID, also known as post-acute sequelae of SARS-CoV-2 infection (PASC), has become a significant public health concern. Among its diverse symptoms, neurocognitive impairments —often referred to as “brain fog”— are increasingly reported by patients long after their initial recovery from COVID-19. These impairments affect attention, memory, executive function, and mental clarity, severely impacting daily life and work.
Research suggests that neurocognitive symptoms in Long COVID may stem from a combination of factors. The virus itself might trigger direct inflammation in the brain (neuroinflammation) or disrupt the blood-brain barrier, leading to cognitive decline. Additionally, the body’s prolonged immune response can cause persistent fatigue, further exacerbating cognitive issues.
To better understand how viral infections, including SARS-CoV-2, affect brain function, research projects like EPIVINF are gaining attention. EPIVINF aims to decode how acute viral infections, such as COVID-19, alter the epigenetic regulation of host factors that are critical for immune control and neurological health. This includes investigating changes in gene expression that may contribute to both immune system dysregulation and the neurological symptoms seen in long COVID. Such research could help pinpoint how viral infections lead to long-term cognitive impairments and offer new avenues for treatment.
In conclusion, neurocognitive impairments in long COVID present a significant challenge. Research like EPIVINF, focusing on the epigenetic effects of viral infections, holds promise for understanding and treating these long-term effects, paving the way for better patient outcomes.