An international meta-analysis, which includes the participation of IrsiCaixa, EPIVINF partner and coordinator, has gathered data from 382 people across 24 international studies to better understand the behaviour of HIV when antiretroviral therapy (ART) is temporarily interrupted in the context of clinical trials.
The study, published in Nature Communications, confirms that post-treatment control, the phenomenon by which the virus remains under control without medication, is very rare, but more frequent in people who start ART shortly after diagnosis. The meta-analysis revealed that, on average, viral load rebounds 16 days after stopping therapy, but a small percentage of the study participants achieve post-treatment control. This control consists of keeping the virus at very low levels in the blood for at least 84 days without antiretroviral drugs. Specifically, only 4% of participants managed to maintain this control; this percentage increases to 6% for people who started treatment within the first six months after acquiring HIV and decreases to just 1% for those who received a diagnosis and started antiretroviral therapy later.
In addition to early treatment initiation, another key factor in promoting post-treatment control is maintaining high levels of CD4+ T cells, which play a critical role in the immune response against HIV.
Exploring the mechanisms behind post-treatment control
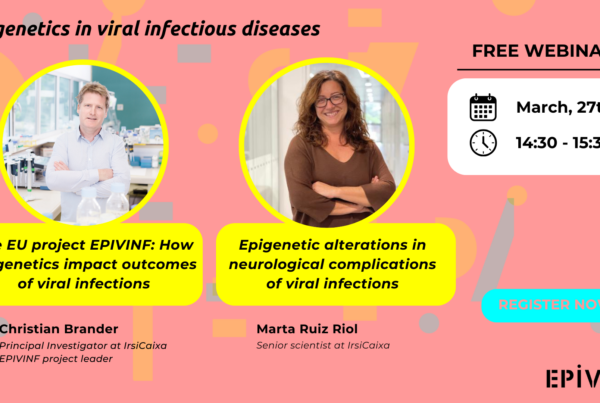
“At EPIVINF, we are particularly excited about these findings, as they include data from participants in the BCN03 clinical trial, who are now being analysed as part of our project. Our aim is to explore how the viral rebound kinetics observed in these individuals may be influenced by their epigenetic signatures and immune receptor repertoires”, says EPIVINF coordinator and author of the study, Christian Brander. Both parameters are being investigated to understand their role in the response to the virus and to assess whether they could be modulated through therapeutic vaccination strategies.
Implications for the design of clinical trials and future therapies
“The study provides essential tools for designing more efficient and safer clinical trials, reducing the number of participants needed for each study, optimizing resources, and minimizing risks for participants“, comments Beatriz Mothe, study author, physician, and researcher at IrsiCaixa. At EPIVINF, this knowledge is fundamental to advancing personalized strategies based on epigenetic and immune profiles, enhancing the chances of success in the quest for a functional cure for HIV.