Scientists are investigating how epigenetic mechanisms, which regulate gene expression without changing DNA sequences, influence HIV’s long-term effects and how these mechanisms can be targeted to improve treatment for HIV disease
The study of epigenetics aims to understand how gene expression is regulated by mechanisms that do not involve changes to the underlying DNA sequence. In recent years, this field has become a game-changer in many medical fields, including HIV research. While antiretroviral therapy (ART) has allowed many people living with HIV to lead longer, healthier lives, the virus remains a persistent concern to individual health and a global health care challenge.
How epigenetics plays a role in HIV
HIV’s ability to evade the immune system isn’t limited to its direct effects on immune cells. The virus also alters the epigenetic “landscape” of the cells it infects, particularly immune cells like CD4+ T cells. One of the most significant changes is in DNA methylation, a chemical modification that can silence or activate specific genes.
Even though ART can reduce viral loads to undetectable levels in the blood, it doesn’t fully eliminate the hidden viral reservoirs. These reservoirs are critical because they are the source of viral reactivation when treatment is interrupted. This means that while ART controls viral replication, it doesn’t offer a cure since the virus can always bounce back from its hidden, dormant state.
The hope in epigenetic modulation
This is where epigenetic modulation could offer new hope. By targeting the genetic switches that control the virus’s ability to hide, researchers are investigating ways to “wake up” the virus from its latent state. These approaches aim to provoke the dormant virus into replication, at which point it can be more easily targeted and eliminated by the immune system.
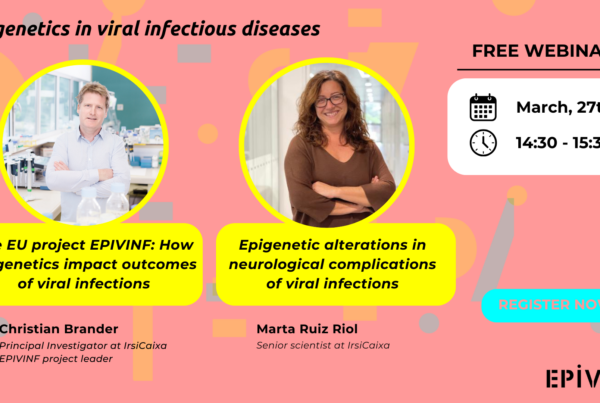
How EPIVINF is paving the way
At EPIVINF, scientists are focusing on how HIV alters the epigenetics of infected individuals. The program will study how changes in the DNA of people living with HIV can affect not only the virus’s persistence but also the person’s immune system’s ability to naturally control the infection. Previous research by IrsiCaixa highlighted that epigenetic differences in the immune cells of people with HIV could influence their immune responses to the virus. These findings suggest that some individuals may have a naturally stronger ability to fight the virus due to these (epi)-genetic factors, guiding ongoing studies at EPIVINF.
By understanding these mechanisms, EPIVINF researchers hope to identify new therapeutic targets. These targets could help control viral replication more effectively, boost the immune response, and ultimately prevent disease progression.